BACKGROUND
Minimally invasive gynecologic surgery offers well-known benefits compared to laparotomy.1 However, laparoscopic surgery requires the development of a distinct skill set that differs from the skills used in open surgery. There is a well-described learning curve for advanced laparoscopy.2 In order to effectively teach laparoscopy to surgeons in training, it is imperative to establish resources used outside of the operating room, which could allow for skill development and improvement in a safe, low-risk environment.
The difficulty of laparoscopic skill development can be overcome with increased exposure and experience during surgical training. However, residents in Obstetrics and Gynecology face unique challenges in obtaining sufficient surgical volumes. These challenges include competing educational demands with obstetrics, decreased cases compared with historical numbers, increasingly complex surgeries being approached laparoscopically, limited work hours, and the need to learn multiple techniques secondary to ever-evolving technology.3 With the identification of these challenges, changes in training programs support the transition to simulator training.4
The role of simulation is to improve psychomotor skill development. Since the introduction of simulation to surgical training, especially within gynecology, several platforms have been developed. Simulators can be of low fidelity, such as a traditional laparoscopic box trainer, or more advanced such as human cadavers or computer-based systems used in robotic simulation.5 Despite the advances and research on simulation, it remains unclear whether simulation education transfers to skills in the operating room or improves clinical outcomes.5 Further investigation is needed regarding which type of simulation and implementation process might correlate with surgical learning.
One of the greatest challenges in laparoscopic surgical training is adaptation to a two-dimensional (2D) view of the surgical field.6 The introduction of the da Vinci Surgical System (Intuitive Surgical, Sunnyvale, CA), a three-dimensional (3D) visual system, has allowed surgeons to augment laparoscopic skills. Although the robotic system provides several advantages that may allow surgeons to feel comfortable tackling more complex laparoscopic procedures, there have been numerous severe adverse events reported from its use and, unlike traditional laparoscopy, it is not fully distributed due to the high cost.6,7 One device that has allowed for laparoscopic surgeons to utilize 3D imaging during surgery with a fraction of the cost of a da Vinci system is the Viking 3DHD Visual System.8 Few reports have evaluated 3D visualization in improving complex laparoscopic gynecologic tasks such as closure of the vaginal cuff during a total laparoscopic hysterectomy.9,10 We aim to investigate whether use of a 3D visual system along with a traditional laparoscopic box trainer for simulation training can lead to improved acquisition of skills on a specific model of laparoscopic vaginal cuff closure when compared with the current 2D visual system and box trainer.
METHODS
This study was approved by the Partners Health System IRB with exemption determination. Initially, eligible participants were current Obstetrics and Gynecology residents at the Brigham and Women’s Hospital (BWH) in Boston, MA. In an effort to increase the number of study participants and due to perceived appropriate inter-specialty cross-over of the topic, eligibility was later extended to General Surgery residents at the Brigham and Women’s Hospital as well. Participation was on a voluntary, non-incentivized basis, and served as consent for the study. A questionnaire was administered to residents regarding level of experience with laparoscopic suturing and future career interests. Study participants were randomly allocated to one of two study arms; utilizing 2D vision or 3D vision during the suturing task. Randomization was performed using the web site randomization.com (http://www.randomization.com) using the method of randomly permuted blocks.
A vaginal cuff model was created (Simulation, Training, Research, Technology Utilization System [STRATUS] center at Brigham and Women’s Hospital, Boston MA) using a metal baking sheet, liquid latex and vegetable spray.11 The cuff model was placed inside a Storz SZABO-BERCI-SACKIER laparoscopic box trainer. For suturing, participants utilized 0 polydioxone bidirectional 28 cm barbed suture on a 36 mm half circle taper point needle which was cut in half and with a pre-tied knot at the distal end of each half. As previously described,11 an initial grading tool was constructed based on a literature review, as well the authors’ own perception of what are important criteria for assessing vaginal cuff suturing in a simulation model. This grading tool (Appendix A), comprised of a checklist and a global rating scale component, was further modified after going through a four-step Delphi validation process (face, content and discriminate validities, as well as assessment of both inter-rater and intra-rater reliabilities). The tool was piloted on five medical students and five expert gynecologic laparoscopic surgeons to confirm that it was realistic for the task of vaginal cuff suturing.
Each participant completed five trials of suturing the vaginal cuff after receiving brief introduction to the procedure. Cuff closure entailed a single layer closure in a running fashion. Every trial was recorded, and then graded independently by two out of the six graders (SCR, EM, MA, HH, DS, JE), using the grading tool described above. Trials were limited to a maximum of 15 minutes. All graders are experienced minimally invasive surgeons, either in Gynecology or General Surgery, and were blinded to identity and proficiency level of the participants.
Fisher’s exact tests were utilized to compare participant characteristics by successful completion of the task and by visualization group and to compare task success between groups. Unpaired t-tests were used to compare the times needed to complete the task at the 1st, 5th and change from 1st to 5th attempt between visualization groups. To compare differences between groups for the global rating scale and checklist scores, we used generalized estimating equations to account for the multiple ratings per subject.
RESULTS
Twenty-five subjects completed this simulation study, 84% of whom were Obstetrics and Gynecology trainees with the remainder being General Surgery trainees. A total of 13 residents (52%) were randomized to cuff closure with the 2D vision system, while 12 (48%) utilized the 3-D system. Table 1 delineates baseline characteristics, exposure to prior laparoscopy and area of career interest by randomization group. Twenty three out of 25 (92%) participants had performed 2D laparoscopy during their residency training. Eighteen out of 24 (75%) participants had never utilized a 3D system before, and six participants (25%) had performed fewer than ten cases with the 3D vision system. The only baseline factor associated with satisfactory completion of both first and final attempts at vaginal cuff suturing within the time limit was prior experience with laparoscopic surgery (data not shown).
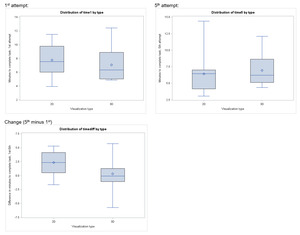
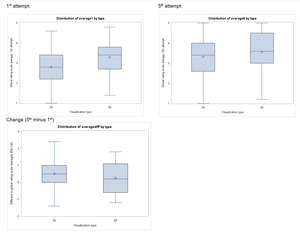
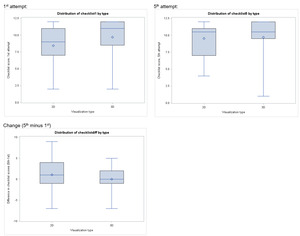
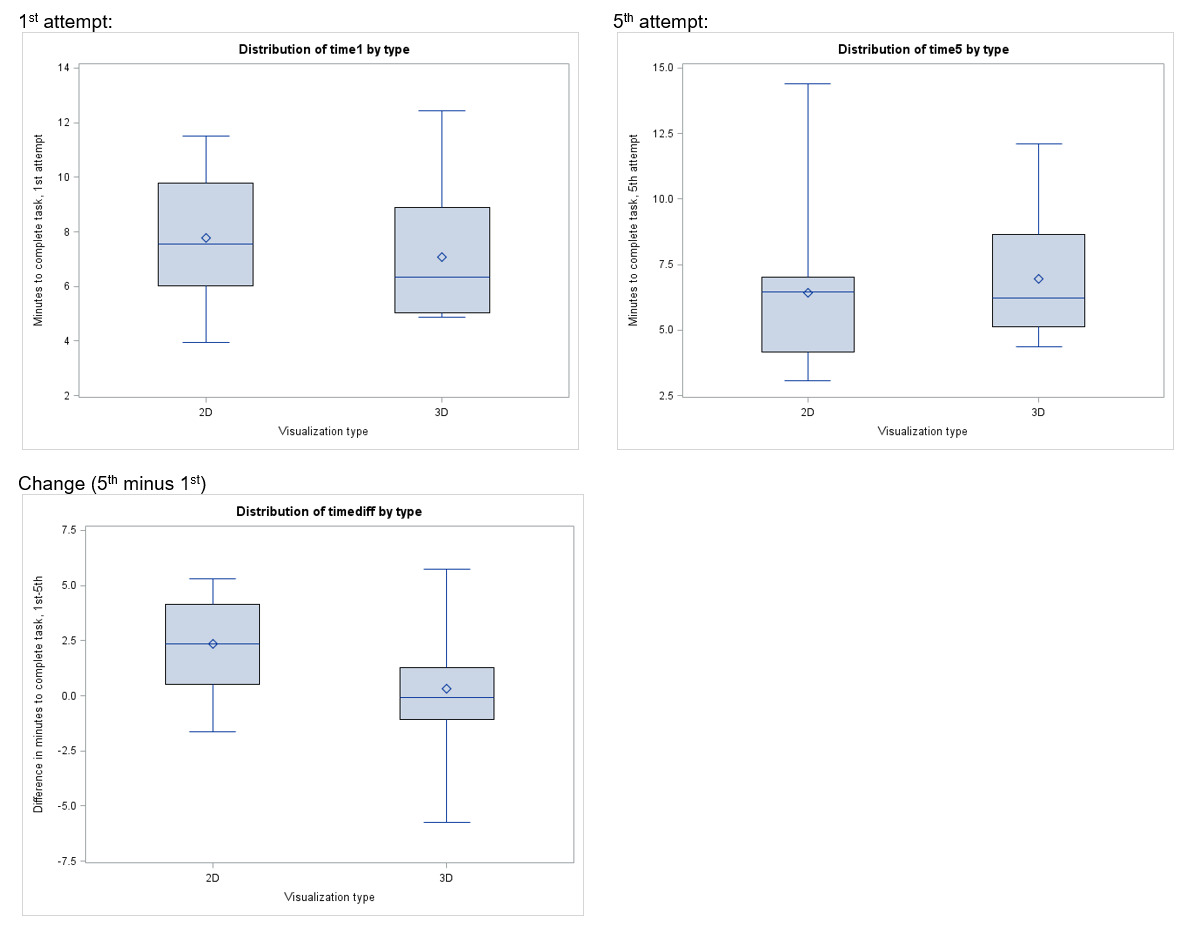
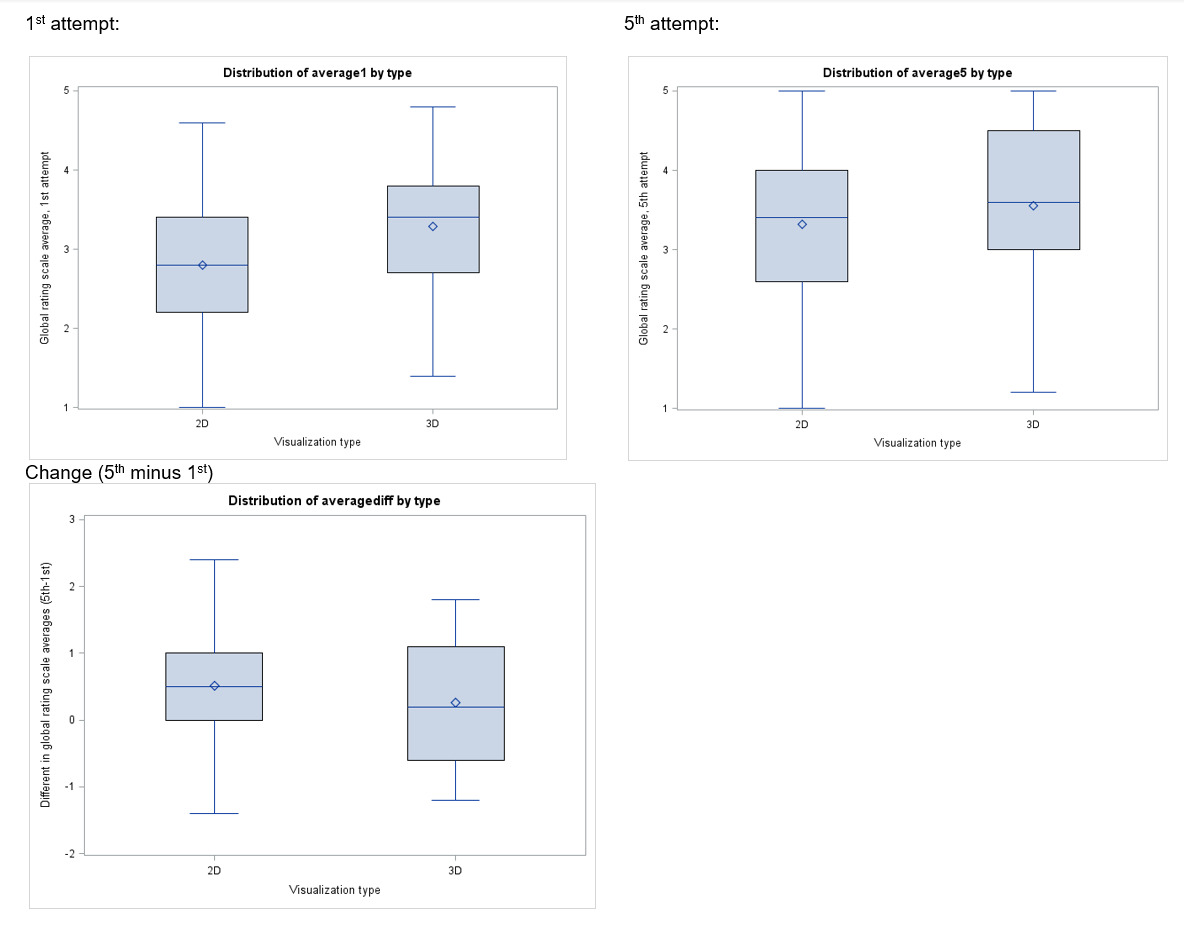
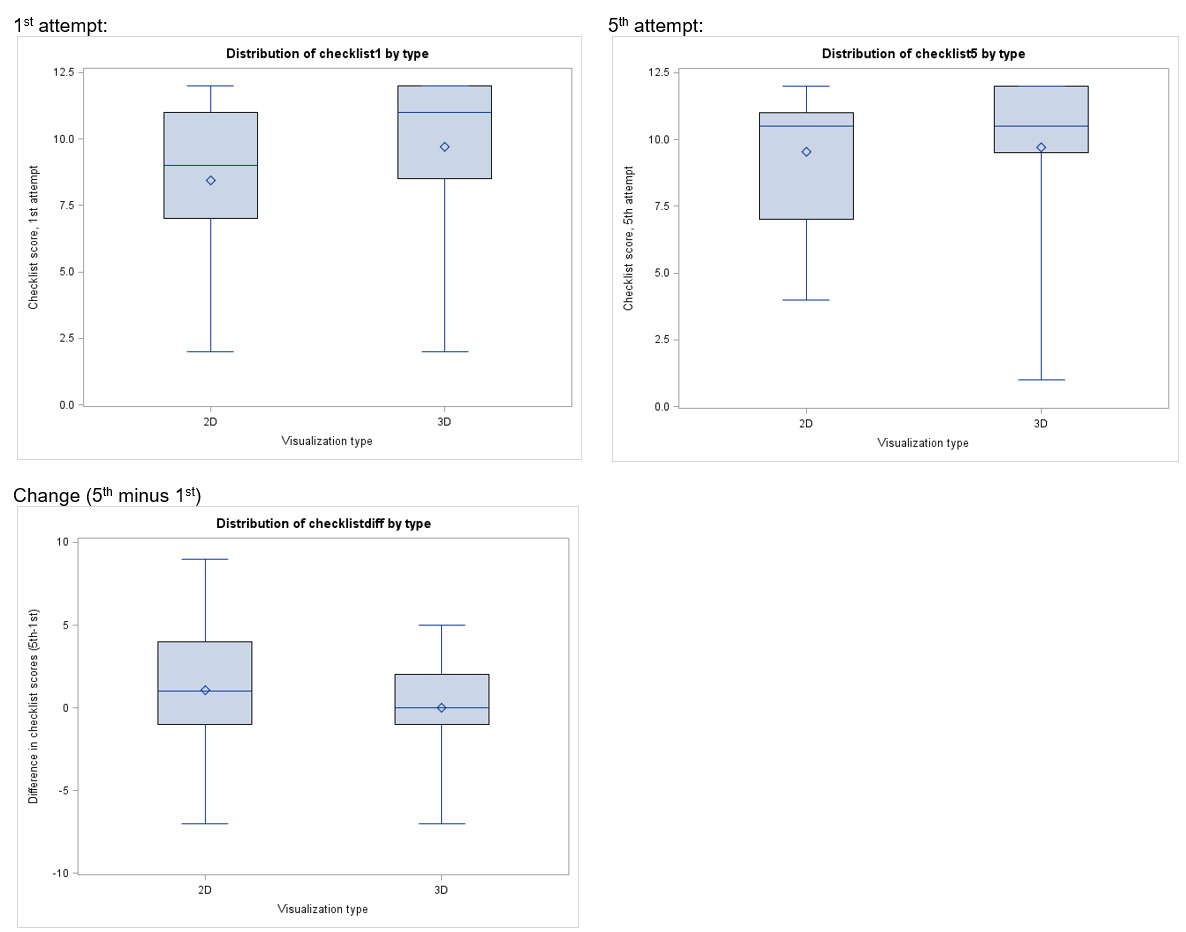
Eleven participants from each arm (85% in 2D, 92% in 3D) completed their first attempt in the allotted time. All participants completed their fifth attempts in the allotted time. Mean vaginal cuff closure time was not significantly different in the first attempt (7.8 min for 2D versus 7.1 min for 3D; p=.49) nor the fifth attempt (6.4 min for 2D versus 7.0 min for 3D; p=.64) based on visualization type [Table 3]. Scores on both the global rating scale [Table 4] and task checklist [Table 5] did not differ significantly by visualization group, although numerically higher scores were noted in the 3-D group. There was minimal and insignificant improvement in minutes to completion (3D, 0.32 and 2D, 2.34 minutes; p= .39), global rating scores (3D, 0.3 and 2D, 0.5-point change; p= .39), checklist scores (3D, 0 and 2D, 1 point change; p= .19) between the first and fifth attempts in each arm.
DISCUSSION
In this randomized trial, the time taken to close the vaginal cuff and the assessment of cuff closure technique was similar with 2D and 3D vision systems. Additionally, over five attempts there was no change in closure time or ratings in either group. There was a trend toward higher ratings in the 3D group, however this was not significant.
There are limited studies comparing 2D to 3D conventional laparoscopy in gynecologic surgery, with variable reported outcomes. Similar to this study, Ko et al conducted an RCT comparing 2D to 3D simulated laparoscopic tasks.10 Although the tasks were more basic and a validated assessment tool was not used, they did find 3D vision was associated with significantly faster laparoscopic suturing. In addition to simulation studies, in-vivo assessments also have conflicting results. In a retrospective study, 3D vision was found to have significantly shorter operating times compared to 2D.12 However, in a prospective study by Ajao et al , there was no change in time trainees required to close the vaginal cuff with 3D vision compared to 2D vision.9
The current study was the first to utilize 3D vision in a simulation setting for an advanced laparoscopic skill specific to gynecologic surgery. We did not demonstrate any benefits of 3D vision over traditional 2D vision for completing a simulated conventional laparoscopic vaginal cuff closure. This finding differs from prior studies on the benefit of 3D vision, including trials of novice urologic and general surgeons completing basic laparoscopic skills.13,14 The lack of identified difference between the two groups in our study could be related to several factors. First, it has been suggested that novice trainees benefit most from simulation practice.5 More than 50% of the participants in both groups were PGY3 and above, nearly 50% of participants in had participated in more than 50 laparoscopic cases and more than 50% of the participants had closed at least 6 vaginal cuffs laparoscopically; therefore, this participant cohort may have been too experienced to demonstrate marked differences. Second, this study suffered from difficulty recruiting a large number of subjects, a common challenge for educational projects when appropriate subjects are limited in number and by time constraints. To help offset this concern, the study group was expanded to include General Surgery trainees as well, however it is possible that this increased heterogeneity in training experiences diluted our findings. Despite the expanded recruitment, there remains a possibility of type II error with this study.
The strength of the study is the use of a validated grading tool that incorporated both a checklist with critical portions of the task as well as a global assessment tool. Additionally, participant randomization and blinding of the assessors adds to the strengths of the study design. The study is also generalizable to a variety of training settings as the simulation design utilizes a very common box trainer set-up that most programs own. The mixture of both General Surgery and Obstetrics and Gynecology trainees as well as varied years of experience may represent a limitation as discussed above. Additionally, the broad range of prior trainee experience may limit ability to detect differences in initial skill acquisition. It has also been suggested that some individuals are unable to perceive 3D imaging on a screen and therefore this type of enhanced simulation will not benefit all learners.9 Although this is rare, participants were not screened for this prior to inclusion. Lastly, participants had minimal prior experience with 3D systems (100% of participants had been involved in 10 or less 3D system surgeries) and this was their first encounter with 3D vision in conventional laparoscopy. The learning curve to operate with 3D vision is unknown and may influence these results.
Conclusions
The use of 3D vision at the time of laparoscopic simulation of vaginal cuff closure did not improve task completion time or technique rating. Although 3D vision does not appear to significantly impact the development of cuff closure skill in this cohort, it may assist a more novice cohort. It is imperative that ongoing advances in conventional laparoscopic simulation be trialed given the importance of skill safety and efficiency. Furthermore, trainees have declining exposure to conventional laparoscopy due in part to the growth and popularity of the robotic system. Thus, simulation training out of the operating room is critical for optimizing learning experiences in the operating room.