Background
The benefits of microincision cataract surgery via a 1.8mm incision have led to increased adoption of this technique worldwide. The major advantage of this technique is reduced surgically induced astigmatism (SIA).1 This allows more predictable surgical outcomes, the ability to achieve more precise refractive aims and ultimately more consistent visual outcomes for patients.
Coaxial microincision surgery uses a main incision size of 1.8mm, compared to a standard main incision size of 2.4mm to 2.75mm used in conventional coaxial phacoemulsification cataract surgery. Mastering the microincision technique requires familiarity with different instruments and variations of techniques compared to conventional phacoemulsification surgery. We are unaware of any previous studies on the safety of teaching coaxial microincision surgery to ophthalmic trainees. The aim of this study was to analyse the complication rates of coaxial microincision cataract surgery performed by trainees, and compare these results to previously published complication rates of trainees performing conventional cataract surgery.
Methods
The records of all 645 microincision cataract surgeries performed between January 2012 and May 2016 at The Queen Elizabeth Hospital, Adelaide, Australia were reviewed. All surgeries were performed by one of either 12 trainees in their third and fourth (senior) years of ophthalmology training in the official (four years of supervised training followed by subspecialty fellowship) training program of the Royal Australian and New Zealand College of Ophthalmologists (RANZCO); three fellows undertaking their fellowship in cataract and refractive surgery; or one experienced consultant cataract surgeon (MG). All trainees and fellows were proficient in performing cataract surgery via a standard sized main incision and were assessed as being capable of operating independently during the study period. All surgeries performed by trainees were under direct supervision of a consultant surgeon.
Ethical approval was obtained for this study from the Human Research Ethics Committee of the Central Adelaide Local Health Network, and the study was conducted in accordance with the Helsinki Declaration. At the time of surgery, information including the surgeon, surgical technique, type of IOL implanted, and any complications were logged in an electronic database. The operation notes of all patients recorded as having had microincision cataract surgery were reviewed to verify that only microincision cases were included in the study. Microincision cases were confirmed by documentation of the use of an appropriately sized keratome for the main incision and from the measurement of the internal wound diameter at the conclusion of the surgery.
Two complications were excluded from analysis as they occurred due to equipment failures completely unrelated to the surgical technique. One of these was a complication in a consultant case in which an IOL haptic was damaged during loading into an injector, and the other was a capsular tear in a trainee case that occurred due to a cannula manufacturing error.
All surgeries were performed in the same manner as taught by the consultant surgeon (MG). Potential variations from standard cataract surgery include: (1) creating a capsulorhexis with a cystotome needle rather than using forceps; (2) smaller phacoemulsification tip and sleeve size with a tight fitting wound requiring wound manipulation and fluid reflux for insertion into the eye; (3) using a second instrument to steady the globe while moving the phacoemulsification probe; and (4) implanting the intraocular lens (IOL) using an incision-assisted technique with a second instrument for counter-pressure. While these techniques may be used with conventional cataract surgery, they are required for such microincision cases.
Clear corneal incisions were made using a microkeratome. 643 of the 645 cases used a temporal incision, and the remaining two used a superior incision. All incisions were measured at the conclusion of the case and ranged in size from 1.8mm to 2.0mm. Three surgeries were performed in conjunction with planned intravitreal injection for the prophylactic treatment of diabetic maculopathy. During the four year study period there were various phacoemulsification machines used due to upgrades in technology and surgeon preference but the vast majority of cases were performed using the Bausch & Lomb Stellaris (Bausch & Lomb, Rochester, USA). Monofocal spherical IOLs were implanted in 69% of cases, monofocal toric IOLs in 24% and multifocal IOLs in 7%.
The occurrence of an intraoperative complication is multifactorial and depends on many variables other than the surgeon’s experience level. In order to account for patient factors which may increase the likelihood of complications, the validated Muhtaseb risk score (M-score)2,3 was calculated for all complicated cases as well as a random sample of 100 uncomplicated cases. The Muhtaseb scoring chart for estimating pre-operative risk of intraoperative complication (Table 1) categorises patients into groups based on scores where 0 = no added risk; 1-2 = low risk; 3-5 = moderate risk; and 6+ = high risk. M-scoring was performed independently by two investigators (EH and BL) using information gathered pre-operatively. There were no inter-investigator differences in M-score assigned to any patient. The random selection of uncomplicated cases was performed using a random number generator.
Results
Microincisional cataract surgery was performed on 645 eyes of 466 patients. Surgery was performed on one eye at a time with a minimum of six weeks between eyes if both eyes were to be operated on. Overall, intraoperative complications occurred in 26 cases (4.03%). The complication rate of consultant cases was 3.16%, the three fellows had a combined overall complication rate of 6.39% and the 12 trainees had a combined overall complication rate of 2.13% (Table 2). There were no significant outliers in complication rates within the group of fellows and trainees.
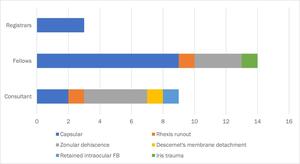
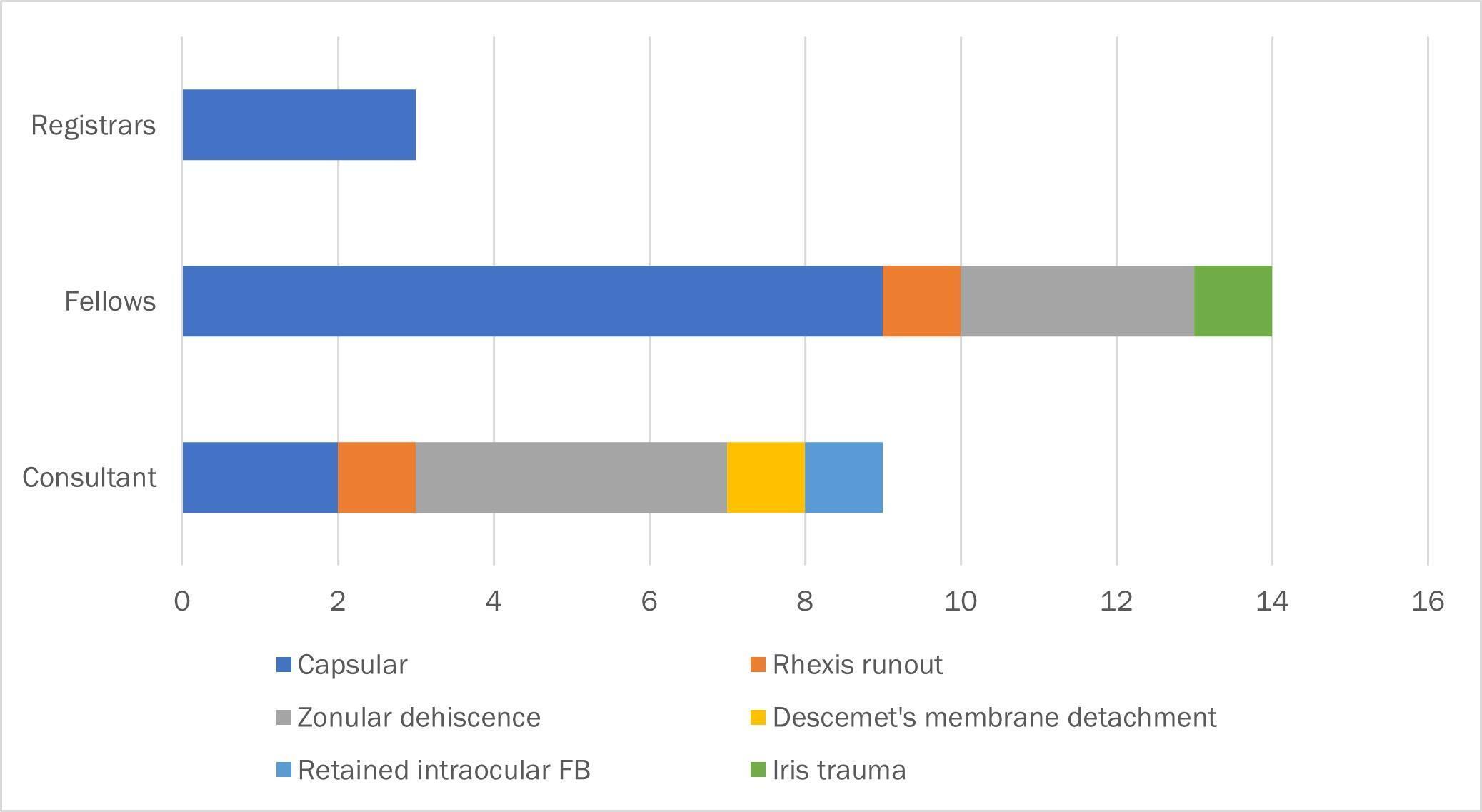
The most common complication (14 of 26) was capsular tear of various types with zonular dehiscence being the next most frequent complication (7 of 26). Other types of complications occurred infrequently. There was considerable difference in complication type distribution between surgeon experience levels (Figure 1).
In consultant performed cases, zonular dehiscence was the most commonly encountered complication and accounted for 44% of complications. In contrast, the most common complication for fellows and trainees was capsule tearing (64% and 100% of complications respectively).
Published studies of complication rates in trainee-performed cataract surgery tend to focus on posterior capsule complications.4,5 To facilitate comparison with these studies, cases of posterior capsule rupture (PCR) with or without vitreous loss, and anterior-to-posterior capsule tear with or without vitreous loss, were grouped together as PCR (see Table 2).
Of the 179 patients who underwent microincision cataract surgery on both eyes, nine had a complication in one eye and one patient had a complication occur in both eyes.
M scores (see Table 1) were calculated for all intraoperative complications (Table 3). The average M score across all complicated cases was 2, which is considered low risk (see Table 1). The average M score for posterior capsule complications was 2 for both consultant and fellow complications and 0 for registrars. For cases in which zonular dehiscence occurred, the average M score was 3 for consultant and 1.3 for fellows. The average M score for a random sample of 100 non-complicated cases was 0.87. For all levels of surgeon experience, the average M score for complicated cases was higher than the average M score for non-complicated cases. Using a Mann-Whitney U-test, for all surgeon levels of experience, complicated cases had on average a statistically significantly higher risk score (p=0.026).
Overall, the risk of complicated surgery was increased 1.3 times for each additional unit increase in the M-score (p<0.001). After adjusting for pre-operative risk (M-score), there were no statistically significant differences in complication rate by status of surgeon, although Fellows tended towards having a higher rate than Consultants (p = 0.075).
Discussion
Complication rates for trainees performing coaxial microincision cataract surgery in our study (2.13%) are comparable with published complication rates for trainees performing standard incision size cataract surgery (Table 4) and were superior to the complication rate (12%) published for trainees performing bimanual microincisional cataract surgery.6
The overall complication rate (4.03%) and overall PCR rate (1.86%) in the current study compare favourably with recently published audit data of all cataract surgeries performed by consultants, fellows and trainees at our study facility (6.4 and 2.59% respectively).21
It is important to note that the trainees included in this study were in their third and fourth year of training, and so would be expected to have favourable complication rates when compared with populations which may include less experienced operators.
We limited our review of previous publications to those published within the last 10 years in an effort to facilitate comparison in terms of equivalent technology and procedures. Included within this literature are several large and national scale audits.4,5,9
It was reassuring to observe that complicated cases in our study had a significantly higher average pre-operative M-score than the sample of non-complicated cases for all levels of surgeon experience. This indicates that complications were occurring due to influence of patient related factors rather than surgical experience or microincisional technique. Generalising the association of M-score and risk of complications, it may be possible to allocate higher risk cases to a more experienced surgeon in an attempt to further reduce complication rates. A recent prospective study of 500 cases has found that allocating all cases with M-scores of >3 to a consultant surgeon was associated with a significant reduction in intraoperative complication rate.22 The M-scores for the sample of non-complicated cases suggested that the consultant is operating on cases with a higher risk score than fellows and registrars, suggesting that an informal risk-stratification process is likely already in effect. We hypothesise that the lower than expected complication rates for trainees performing microincision cataract surgery may have been partly due to a combination of informal risk-stratifying and case allocation between supervisor and trainee during operating lists, as well as increased supervision of trainees performing surgery.
In our study facility, the majority of standard cataract surgeries (60.5%) are performed by trainees, and are most commonly under direct supervision by a consultant.21 In contrast, the majority of microincision procedures (78.1%) were performed by a consultant or fellows. A large part of this difference is that the supervising consultant (MG) is the only consultant at our facility to employ a fellow and one feature of the fellowship is to gain competence with microincision cataract surgery.
The higher complication rate for fellows was to be expected, as anecdotally these operators are expected to be tackling more complex cases due to the nature of their cataract and refractive surgery fellowship. However, M-scores for the uncomplicated sample of fellow cases was lower than other groups, not supporting this observation.
Conclusions
Our results indicate that trainees are safe to be taught to perform microincisional cataract surgery via a 1.8mm incision. All trainees in this study had previously gained competence with standard cataract surgery prior to moving on to this more advanced technique. Their lower than commonly reported complication rates suggest that microincision techniques can be taught safely once competence at standard techniques has been demonstrated. In fact, there were no trainee cases complicated by iris trauma or capsulorhexis runouts, which may indicate that the more stable, tighter-sealed anterior chamber offers better stability and a safer environment to operate in.
Giving trainees the skills to access the benefits of the microincision technique, may help them prepare for their future careers in the knowledge that there is a constant downward trend in incision size over time. Ultimately, teaching trainees to use a technique they are likely to use after becoming consultants is likely to decrease complication rates and help improve visual outcomes for patients.