Introduction
Coronavirus disease 2019 (COVID-19) has incited a global emergency that presents numerous challenges for health care worldwide. An often-overlooked aspect of this disruption is that on medical education.1 The impact on undergraduate medical student on clinical placements and clerkships has proven most conspicuous with the alteration, and even cancellation, of student clinical rotations.
Undergraduate general surgical education is traditionally delivered through didactic lectures and direct observation on clinical placements.2 Thus, pedagogical models of surgical education rely on role modelling and ‘hands on’ clinical experience.3 Teaching modalities have evolved significantly with technological advancement supplementing traditional lectures and enhancing self-directed learning.4,5 Thus, a variety of traditional, web-based and interactive visualisation tools are utilised in general surgical education for both surgical trainees and medical students.
The arrival of COVID-19 has urged academic communities to adapt and establish forward-thinking, practical and adequate methods of surgical teaching in place of usual clinical placements. As such, enduring transformative approaches to surgical methods of teaching have never been more imperative. This review sought to identify and summarise the literature related to remote modalities of general surgical education to medical students.
Methods
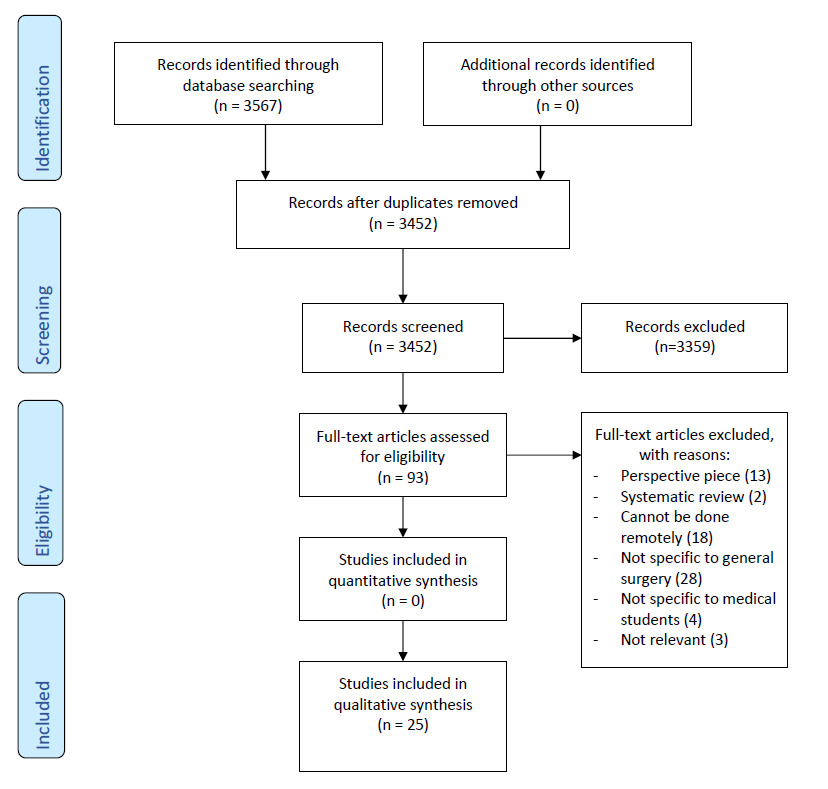
A systematic review was performed as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement where possible.6 All studies that investigated the delivery of remote methods of general surgical education during undergraduate medical student placements were included in this study. For this study, remote methods of surgical education were defined as virtual interactive learning platforms including; videoconferencing, web-based/online and audio (including podcast) forums.
Information Sources and Search Strategies
Electronic searches were performed in PubMed, MEDLINE, Embase and Cochrane Controlled Register of Trials (CENTRAL) from inception to December 31st, 2020. Following a brainstorm session, two authors (JR and BO) collated a list of keywords to build search strategies for each database (Table 1). Study design or language limitations were not applied. Search results were downloaded and managed with EndNote X9 citation manager (Clarivate Analytics, Philadelphia, PA, USA). Reference lists of all included papers was performed to retrieve any texts that may have been missed in the initial search. The last search was performed on April 4th, 2021.
Study Selection
Two reviewers (CX and BO) independently performed the searches and examined titles and abstracts to exclude irrelevant reports and produce a list of studies for full-text review in an iterative manner. Studies were initially excluded if they were published in languages other than English, if full texts could not be retrieved (i.e., conference abstracts) and if they were perspective pieces. Following this, two reviewers (CX and BO) screened eligible studies applying the following criteria: 1) studies involving medical students only; 2) studies describing general surgical education pedagogies and 3) studies describing remote modalities of surgical education (i.e. online or self-directed modalities).
Data Abstraction and Analysis
An electronic data extraction sheet was developed in Microsoft Office Excel 2019 for all included studies. Two authors (CX and JR) extracted data from the included studies. This was pilot-tested on the first three studies and finalised for subsequent articles. Both authors subsequently proofread each other’s datasheets and reconciled any differences. Data extracted from the included studies included 1) study characteristics (journal, setting, exposures and comparisons and sample sizes) 2) outcome measures and 3) study conclusions.
Data Analysis
A qualitative synthesis methodology was employed to analyse all included studies by two independent reviewers (CX and JR).7 An inductive approach to thematic analysis was performed where all studies were read several times and manually coded and grouped into themes.8 Initial codes were generated, revised, inspected and grouped appropriately into themes. Themes were named, defined and compared. Final readings of all articles were performed to contextualise the themes and to ensure study relevance and applicability.
Results
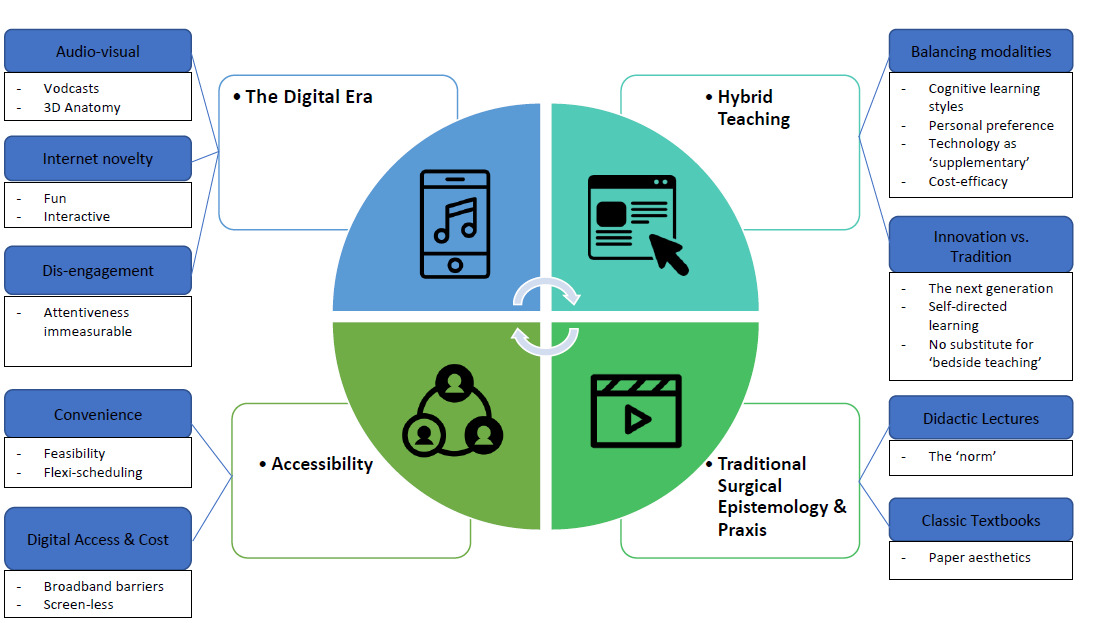
Of 3566 records identified in our initial database search, 25 articles were included (Figure 1). The study characteristics of all included articles are summarised in Table 2. Four major themes were identified following inductive thematic analysis of all included studies. Figure 2 presents a flowchart depicting the major themes, sub-themes and primary codes leading to their development. Qualitative descriptions of each theme are presented in detail below.
Theme 1 – Hybrid Teaching
The first major theme identified and most prominent across all studies centred around the concept of blending traditional and innovative technology-based modalities of teaching. Studies sought to balance teaching modalities in their curriculum leading to the common code of ‘technology as a supplementary tool’ among half of the studies.9–19 For example, Devitt et al. (1998) acknowledged that computer-based learning supplemented clinical teaching by exposing students to a greater diversity of cases.14 Studies also acknowledged that surgical education pedagogy needed to consider personal learning preferences,9,12,20,21 cost-effectiveness,15,22 and cognitive learning styles.9 The subtheme of innovation vs. tradition highlights an ongoing conundrum for medical educators to evolve medical education at the pace of a next generation of more proficient technology users. This is further exemplified by a push for a more self-directed learning approach,16,17,23–27 hereby encouraging independence whilst acknowledging that remote education is still limited as a substitute for bedside teaching.9,10
Theme 2 – The Digital Era
Another theme that was evident across all studies was that of ‘The Digital era’. Audio-visual aspects of remote learning tools that were studied primarily involved the use of vodcasts19,25–28 and 3D anatomy programs.15,18,29 Using the internet as a teaching modality was deemed as novel and hence was a prevalent subtheme. Among the included studies, positive reactions from students were reported with students describing digital surgical education forums as a ‘fun’ approach to learning when compared to traditional methods of teaching.11,12,14,15,19,20,30 Several institutions initiated internet-based interactive simulations to mimic clinical experiences.16,19,22,31 Whilst the overwhelming majority of studies supported the addition or enhancement of a digital curriculum, consideration of the potential for dis-engagement and personal accountability was noted in remote settings.10,11,14,22,27 Overall, studies reporting digital surgical pedagogy advocated for digital modalities to be incorporated into current curricula whilst still acknowledging traditional theory and praxis. This intersected with the theme of ‘Hybrid Teaching’ where a constant link with traditional lectures, bedside teaching and self-directed textbook learning was maintained despite access to novel technological teaching modalities.
Theme 3 – Accessibility
Accessibility was a major factor that contributed to the appeal of remote surgical education. A shift to an interactive, multimodal curriculum has been observed.32 Student responses to several different modalities reported feasibility due to their ease of use and practicality.15,16,28,31,33 Studies such as Kumar et al. (2011) utilized laparoscopic recordings that were readily available from laparoscopic surgeries at the hospital to provide teaching modules.15 Flexibility in scheduling remote teaching curricula make it easier to promote a self-directed learning approach.10,14,16,18,24,31
A challenge to implementing new tools is the digital access and cost barriers that can affect both students and institutions. Broadband requirements were once a barrier for students but have now largely become a concern of the past, predominantly within developed countries. However, this does not mean that costs are easily alleviated for the current generation of medical students. Harrington et. al. (2018) investigated the use of virtual reality headsets for immerse 360-degree operative videos as a substitute for in person attendance.22 The use of this technology is still novel. Nonetheless, it is still important to celebrate how digital technology has alleviated faculty costs and other barriers through reducing staffing and resource barriers.16,17,24,26
Theme 4 – Traditional Surgical Epistemology and Praxis
Studies sought to compare new techniques to traditional surgical pedagogies. As mentioned previously, didactic lectures traditionally comprise the bulk of medical student teaching.9,12,16,17,28,31 Two studies also noted that traditional didactic lectures and classical textbook-centered learning was reported to be favored by students for their paper aesthetics.12,18 Both of these tools had been used within the control groups and produced a recurring sub-theme of that there were a continuing divide amongst students’ preferences for either a traditional or modern teaching methods.12,18,33 Overall, whilst studies examined modern technologically advanced modalities for surgical teaching, these were always considered an adjunct to customary teaching practices.
Discussion
Surgical education for medical students largely involves lectures and hands on experience through clinical placements. Amidst COVID-19, traditional face to face lectures and tutorials have transitioned to virtual forums with clinical placements suspended or shortened limiting opportunities for student-patient interactions. This review sought to identify and summarise remote methods of general surgical teaching for medical students that could be feasibly instituted amidst COVID-19 disruptions.
Studies reporting technological advancements in surgical education for medical students have largely emerged within the last two decades. The use of computer-based software programs and video-conferencing mediums that, while novel and innovative for their time, are beginning to feature regularly within medical school curricula. It has been asserted that the transition to online platforms should be critically examined due to adverse risks on medical student acquisition of knowledge and clinical skills.32 However, the COVID-19 pandemic has created opportunities for innovation within digital forums for delivering medical education.
Prior to COVID‐19, a shift away from didactic learning and towards self‐directed, team-directed and/or case‐based learning was already in motion.34 Internet-based education modules have been modernized with the introduction of interactive clinical simulations, computer-based clinical examination assessments, interactive surgical skills training videos and video-conferencing.35,36 Not only do these tools allow for the remote supplementation of additional hospital and surgical skills experience, students may appreciate that such methods are beneficial for self-directed learning approaches.17
Online teaching tools and forums optimising the delivery of medical education are now able to be developed reasonably quickly. The challenge will now lie considerably with providing adequate support for the implementation of these resources in conjunction with student experiences and feedback.32 Currently, institutions have been exploring more innovative and immersive methods of remote surgical teaching. Several studies utilized virtual reality as an educational tool to build on the pre-existing concept of patient simulation programs. In 1999, videoconferencing operative procedures for students’ learning was initially trialled.11 Whilst novel for its time, current technology has vastly improved this approach with virtual reality headsets now providing an immersive 360-degree view of laparoscopic surgery.22 There is potential for VR to revolutionize the future of surgical teaching by creating a fully immersive simulation of the ward and even real-life patient-based experiences.
Remote learning tools such as those described in this review are practical and allow flexibility in academic scheduling for students. This offers a choice for students to adjust these resources to their personal learning style and facilitate learning at one’s own pace. This ‘work-from-home’ concept has become common practice amidst COVID-19 with an emphasis on self-directed learning.27 Despite this, students have indicated a preference for traditional teaching modalities.12 Thus, the theme of incorporating hybrid teaching models acknowledges the importance of traditional epistemology and praxis in surgical education.
There are many challenges for academic institutions in implementing nuanced methods of digital medical education. Logistical issues related to internet, software and adequate computer or tablet access have been noted in several studies in this review.11,20 Although these factors have become more accessible over time in developed countries, cost and remote support will continue to pose significant barriers. Additionally, advanced virtual reality technology is an expensive endeavour limiting the ability to accommodate student numbers.22 However, solutions such as utilizing readily available laparoscopic procedures to create educational content have been identified to be cost-efficient and a blended, online curriculum has also been noted to reduce staffing resources required.15,17 Additionally, student isolation and disengagement s another limitation to remote learning. The lack of student-teacher interaction has been shown to decrease student motivation.20 Overall, there is still no real substitute for bedside teaching and interpersonal patient interactions.
There are several limitations to this review. Firstly, this study only included studies that were deemed relevant to medical students undergoing clinical rotations in general surgery. Studies performed within other surgical specialties were not included. This could motivate other researchers to conduct reviews within these specialties to further expand on surgical education pedagogies in the context of the current COVID-19 pandemic. Additionally, given this is a narrative review, the findings of this study are not generalizable, due to study heterogeneity in the methodological design of each included study.
In conclusion, the evolution of medical education is moving towards a more technological enriched environment with the COVID-19 pandemic accelerating this movement to accommodate the disruption of traditional didactic and bedside teaching. This review provides a source by which educators may draw ideas as they continue to transition between remote and traditional methods of general surgical education. It also highlights the numerous tools and methods available to improve the delivery of medical education whilst facilitating supportive and engaging spaces for students to learn from within their own homes. These teaching modalities will continue to be refined, developed and integrated into traditional medical curricula and their evolution over time will improve the ways in which we engage medical students in virtual settings.