INTRODUCTION
Early introduction to surgical skills and practical learning can improve skill acquisition, interest in a surgical career and confidence in formative training years.1 Despite surgical placements forming part of standardised modules at UK medical schools, there is considerable heterogeneity in access to teaching, and indeed to practice surgical skills in simulations or in situ.2 Moreover, literature suggests that dedicated opportunities to learn and hone surgical skills can improve preparedness and reduce anxieties surrounding placement or foundation jobs in surgery.3 We chose to deliver a workshop on K-wiring to undergraduates: it is a technique which is relatively easy to grasp, but with great merit in surgical practice, particularly in fractures of the hand and wrist. K-wiring may be considered an intermediate skill before a trainee may progress to expert skills, and as such early acquisition of good technique may reflect on the trajectory of a surgeon’s career.4
Establishing effective skill teaching during placements may be difficult given the workload and time restraints of many operating departments in teaching hospitals.1 Furthermore, reductions in training opportunities as a foundation doctor or core trainee mean simulation is an increasingly popular means of surgical training. Simulation infers the re-creation of conditions to mimic a real-life scenario: in this instance, the operating theatre. Removing initial skill acquisition from a high-pressure environment with a real patient may allow students better engage with learning as well as operate in a safe environment, without risk to patients. Students will have more time, the opportunity to ask questions and receive feedback in an immersive environment.5 Likewise, it affords surgeons the ability to operate efficiently and demonstrate techniques, whilst also ensuring students progressively acquire skills to translate into real life cases where appropriate.6 This may lead to an increased medical student confidence and positive attitudes of surgery in the short term, and indeed improved performance of surgical skills and likelihood of choosing an operative career longer term.7
To deliver our K-wiring skills course we used a novel 3D printed metacarpal simulator, and a novel 3D printed phalange complex. These simulators consist of an anatomically accurate printed bone cortex, which is hand filled with a different density medullary core. This allows for realistic cortico-medullary differentiation and tactile feedback during drilling when one passes from the cortex to medulla. Previously published results have shown that these simulators are equivocal to real bone and provide a more replicable and useful simulation experience than predecessors.8 The use of 3D printed cortico-medullary differentiated bone was also described by Javan et al, who utilised it as part of a simulated shoulder complex. This re-enforces the use of highly realistic models throughout the various stages of surgical skill acquisition, with specialty trainees still benefitting from repeat practice without increasing burdens on theatre time or patient results.9
The objectives of our study were:
-
To assess whether undergraduate students felt better prepared for surgical placements following an integrative workshop
-
To assess if a cortico-medullary differentiated simulator aided their learning experience.
We theorise that tactile learning of a basic surgical skill (Kirschner-wiring) will aid a student’s preparedness and confidence prior to undertaking surgical placements.
METHODS
Course Aims
-
K-wiring principles and basic techniques
-
Indications for K-wiring
-
Experience of a metacarpal and phalange bone simulator for surgical skills
Study Population
A total of 16 undergraduate medical students attended the workshop, with 62.5% being within pre-clinical years 1-3 and the remaining 37.5% In clinical years 4-5. Only 20% had previous simulated experience with Kirschner wires, and none with Suzuki frames. Inclusion criteria were as follows: undergraduate level, medical student, any previous level of experience with Kirschner wiring, able to converse in English, and able to provide informed consent. Exclusion criteria were limited to students of another healthcare degree and qualified doctors and/or surgeons. This workshop formed part of an optional skills day ran by the medical school’s surgical society, and so each student had volunteered to attend with no formative or summative assessment of performance.
Pre-workshop presentation
The course took place on a single morning, with a stand-alone lecture following by groups rotating through the skill workshop. To provide an initial understanding of K-wiring, a 20-minute lecture was presented. This lecture included a visual presentation demonstrating how to mount their K-wire to the drill and photos of the wiring techniques to be practiced in the workshop. This was in conjunction with a verbal presentation that described the different indications for each technique, and an overview of the simulators with regards to the unique design that would give the students a realistic ‘feel’ when passing through medulla to cortex.
Skill workshop
The skill session lasted approximately 30 minutes for each group of 3-4 students. For our simulator session we allocated a metacarpal and a phalange complex to each student and sequentially taught longitudinal and cross-sectional K-wiring skills and Suzuki frame construction. Each student had a drill, ample K-wires of varying sizes and a board to which they could stabilise their metacarpal. Under guidance they were able to attempt single longitudinal wiring first, receive feedback on their technique and re-attempt until successful. A supervisor then ink marked a fracture line for the student to attempt to cross wire, again repeating the feedback and adapt cycle until they were successful. Depending on the students’ performance thus far they may have had time to practice shot-gun wiring, though unfortunately we found this not to be the case at this skill session. Instead, we prioritised time for students to attempt the Suzuki frame with the phalange complex, which involved two separate transverse K-wire insertions before bending, trimming and banding the wires. All students were able to practice both these skills on once simulator of each kind (metacarpal and phalange each) once within the skill session.
This course utilised two instructors (one registrar level, another a final year medical student) per 3-4 students at a time. Overall, 16 students completed the workshop.
To assess whether the course met our intended outcomes, we asked each attendee to complete two questionnaires. We used a combination of response types, including free text boxes to ascertain previous knowledge and experience with basic K wiring, and open feedback from attendees. For quantitative data, we used a 5-point Likert scale to assess how useful the workshop was, metacarpal ease of use, teaching quality and confidence. An equivocal questionnaire was undertaken for the Suzuki frame workshop using the phalange complex. Of note, these questionnaires were self-reported.
Outcome measures
-
Did students feel more prepared for surgical placements following the workshop?
-
Did students find the cortico-medullary differentiated simulators aided their learning experience?
RESULTS
Sixteen students received teaching on both simple K-wire techniques, and Suzuki frame construction. We found that compared to only a minority having experience or knowledge of either skill pre-workshop, afterwards almost all students felt more confident and skilful.
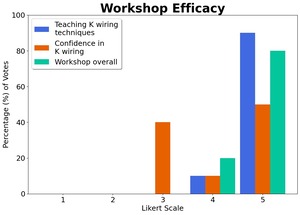
80% of delegates had no previous experience of K-wiring, with 70% of those students unaware of indications for performing K-wiring. Pre-workshop, 80% of students were unaware of the different K-wiring techniques that could be performed. Usefulness of the workshop was rated as 5/5 by 80% of delegates regarding cross K-wiring (Figure 1), with 1 being not useful and 5 being extremely useful. 90% of students also rated the teaching of the workshop as 5/5. We found a greater spread in the students’ confidence in performing K-wiring, with 50% scoring 5/5, 10% scoring 4/5 and 40% scoring 3/5, quite possibly reflecting the variation in previous exposure to surgical skills.
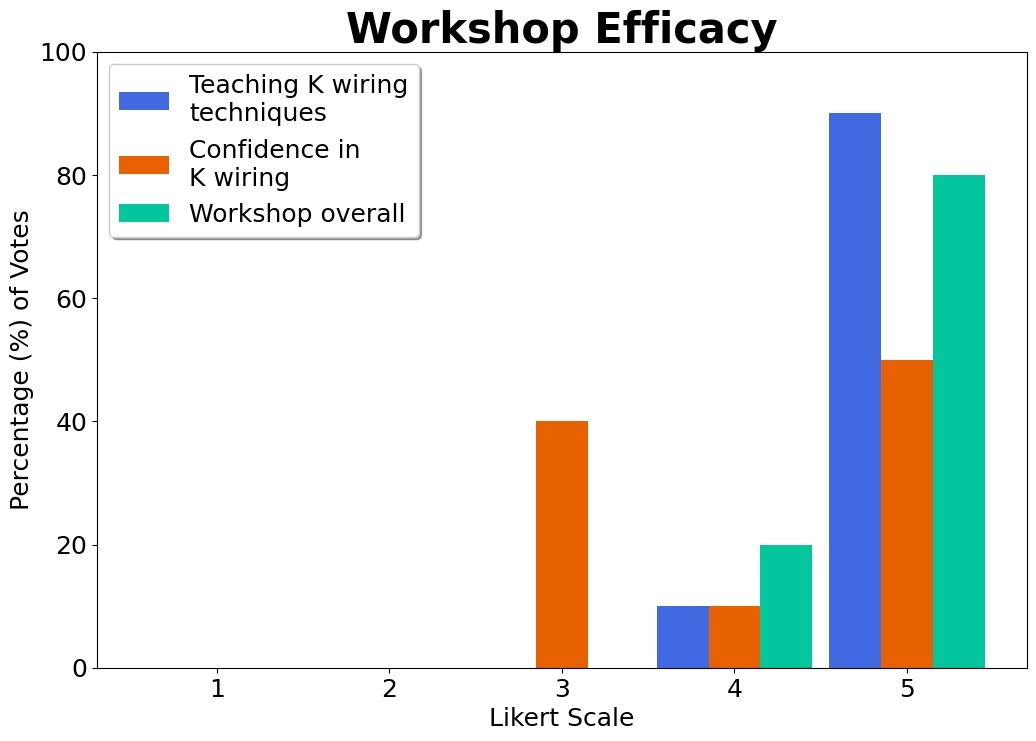
We also asked delegates to score two facets of the performance of our metacarpal simulator, anatomical accuracy and ease of use. For anatomical accuracy, 80% scored it 5/5, with 20% scoring it 4/5. For ease of use, 40% scored it 5/5, 50% scored 4/5, and the remainder scored 3/5 (Figure 2).
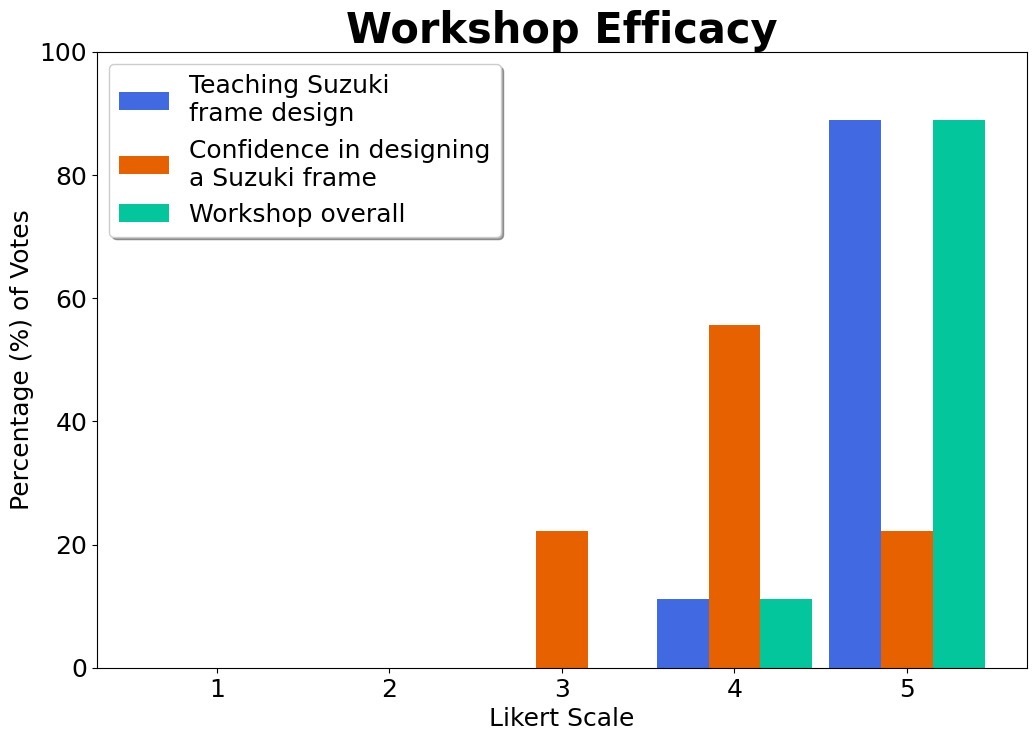
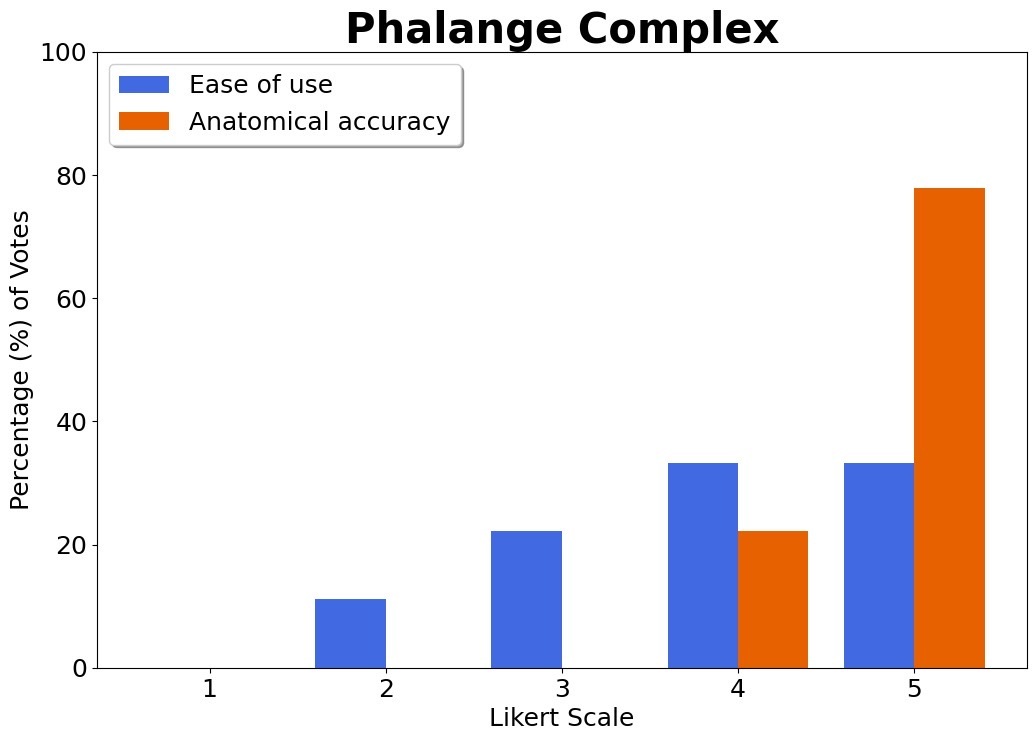
100% of delegates had no previous experience constructing a Suzuki frame. 12.5% had some awareness of indications and the theory of creating one pre-workshop. Usefulness of the Suzuki frame workshop was rated as 5/5 by 80% of delegates (Figure 3). Teaching of the Suzuki frame design and construction was also scored 5/5 by 90%, with the remainder scoring 4/5 for both above outcome measures. Confidence in creating a Suzuki frame was scored 4/5 by 50%, with an even split of 5/5 and 3/5 for the other half of delegates. Regarding our phalange complex as a learning tool, 80% rated anatomical accuracy as 5/5, with 20% scoring 4/5. Ease of use was scored 4 or 5/5 by 60%, with the remainder scoring 2 or 3/5 (Figure 4).
Our metacarpals and phalange complexes were deemed highly favourable by most students (Figure 3 and 4 respectively), with the following free text responses given as feedback for the experience using our simulators. This related to both usability, anatomical accuracy and enjoyment of using the simulator. Responses included “It was a really good demonstration and wasn’t the easiest to use, which makes it better as it’s more in keeping with real life”, I really enjoyed it", “Interesting”, “9/10”.
We also offered free text boxes to give delegates the opportunity to give qualitative feedback on their experience. Some of the responses collected include:
“It was my favourite station so far”
“I really enjoyed it and would like to do more”
“It was excellent”
“Very good”
“Very easy to use”
Finally, we asked students if they had any thoughts on further adaptations to our Suzuki frame simulators that they felt would have enhanced their learning experience. Two responses were gathered:
“Add some blood vessels so we can practice how to avoid them when performing the procedure”
“Add neurovasculature so we can practice how to navigate through that”
We agree that providing soft tissue elements to our simulators would help increase replicability of the skill for students in theatres and strive to offer such in future workshops.
Images 1 and 2 show a visual aspect of the workshop experience.
DISCUSSION
The K-wiring course was highly effective at better preparing students to understand principles and undertake basic K-wire fixation. A particular highlight for students was the use of high-fidelity simulators. For many it was their first experience of using surgical drilling techniques in surgery, and the unique haptic feedback of both the metacarpal and phalange simulators offered them real-time estimation of whether they were passing through cortex or medulla.
Our K wiring course was overall found to be informative, well formatted and of high yield to the medical students who undertook it. To demonstrate the educational advantages of our tutor led bespoke simulator workshop, we utilised a series of questionnaires to assess prior knowledge and experience, and student opinion of usefulness, teaching and enjoyment.
We believe the format of a short lecture to give students a basis of understanding for the indications and technique, followed by small group workshops with immediate feedback, were of great benefit to the learning process. A previous study compared the efficacy of simulator workshops with and without instruction and feedback in 4 groups, with the quarter given both instruction and feedback performing better than peers.10 The groups of 3-4 allowed us to give positive and instructive feedback throughout, allowing students to maximise their use of the single simulator and limited time to achieve the skill they were attempting.
One metacarpal and one phalange complex were found to be sufficient for each student. Delegates were able to utilise the entirety of the slot, and able to independently practice skills with feedback and support from tutors.
We also found the staff: student ratio to be excellent. Being 1:2 at most allowed all students to ask pertinent questions and receive hands on assistance if they struggled completing the skill.
Another feature we found to enhance the workshop was a short preparatory lecture delivered directly before. Given the novelty of the skill and its indications, a series of pictures and overview of basic techniques allowed students to enter the workshop prepared and maximise time for practical skills.
Looking ahead to further courses, there are several areas we can improve training above an already well-resourced and effective course.
A proportion of our students took several repeats of longitudinal K-wiring as they familiarised themselves with the density feedback and the drill itself. This meant although they received the theory teaching on shotgun K-wiring, only a few managed to progress to this skill within the time frame. Having both a longer workshop overall and set times for each skill may help facilitate students achieving all learning targets. Furthermore, lack of previous experience meant some found it difficult to stabilise the metacarpal during drilling. Whilst we improvised on the day with assisting ourselves or the use of pliers to clamp the simulator, a clamp for each student would likely be a better option.
At future workshops, we hope to supply the same method of teaching followed immediately by practical skills to maximise learning and engagement. Following excellent feedback regarding the two simulators trialled we will endeavour to repeat provision of 1 of each per student but facilitate the practical opportunity with more time and a stabilising element of kit to assist novices in drilling safely.
A limitation of this study was the use of two subjective questionnaires and the small study group. To re-enforce our results, we would like to coalesce data from further workshops, collecting comparative data against other simulators for statistical interpretation, and an objective questionnaire to reduce reporter bias.
CONCLUSIONS
We were able to demonstrate a large improvement in medical student knowledge, confidence and skill in a surgical skills course on K-wiring and Suzuki frame construction, using high fidelity novel simulators. Feedback suggests a combined lecture and practical skill session maximised student learning during a short time window and provided both new knowledge and the confidence to attempt the described surgical skills under close supervision. Providing each student with a novel and realistic bone simulator facilitated a realistic feel to the practiced skill, and provoked enthusiasm for surgery as a potential future career.