Introduction
The field of minimally invasive surgery has evolved tremendously over the last decade. Robotic-assisted surgery has increased substantially and is now commonly performed throughout the developed world. However, uptake has increased heterogeneously across a range of surgical disciplines, especially within general surgery and its subspecialties.1,2 Like laparoscopic surgery, robotic surgery offers significant benefits to the patient. It is proven to help with faster recovery and reduce wound complications, bleeding, and pain.3 Furthermore, robotic surgery has several advantages over laparoscopic and open surgery. It offers enhanced precision, flexibility, control, enhanced visualization, anatomic access, better ergonomics, decreased fatigue, and less surgeon tremor therefore facilitating operations.4–6
Several societies, including the leading Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), have published consensus statements emphasizing the need for structured robotic surgery curricula.7 This growing emphasis on standardized training reflects a broader shift toward competency-based approaches in surgical education. However, the use of robotic surgery in Canada has been and remains limited compared to the United States (USA). This disparity is driven largely by the structure of Canada’s single-payer healthcare system, this limitation is the result of the costs associated with procedures, maintenance, and training required without proven substantial benefits as compared to laparoscopic surgery.8
Despite this, robotic platforms are increasingly being adopted for complex procedures such as revisional foregut surgery, pelvic surgery in urology and gynecology, colorectal resections, and abdominal wall reconstruction.9,10 The growing prevalence of robotic surgery in the USA and other parts of the world has led to significant shifts in surgical training. Most general surgery programs there now include longitudinal robotic curricula, often culminating in full robotic certification through Intuitive Surgical.11–14 Many American fellowship programs now expect robotic experience at the residency level. As such, robotic competency is becoming an important differentiator for trainees in both academic and community job markets. Yet, in Canada, formal robotic training programs in general surgery remain scarce.
A recent national survey by Muaddi H et al. of all general surgery residency and subspecialty program directors (PDs) in Canada showed that 75% of PDs indicated access to the robotic surgical system. However, only 33% indicated that surgical trainees are given the opportunity to use the robot platform in the clinical setting. Lastly, none felt that their trainees gained enough competence in robotic surgery to practice independently.15 Unlike in Urology—where robotic integration has been more successful13—Canadian general surgery trainees still depend on ad hoc experiences that vary widely between institutions. Currently, many residents and fellows seeking robotic training must do so independently, often by traveling internationally at personal expense. This model is unsustainable and inequitable. At a minimum, Canadian trainees should be offered foundational robotic education to remain current with global surgical practices, competitive in the job market, and ready to adopt future robotic innovations.
The University of Toronto (UofT) is uniquely positioned to lead the development of robotic education in Canada. The Temerty Advanced Surgical Education & Simulation Centre has prioritized training in robotic-assisted surgery, and Toronto General Hospital—one of the country’s leading academic institutions—has recently acquired several state-of-the-art Da Vinci Xi robotic systems. With these resources in place, we recognized a timely opportunity to pilot a structured, simulation-based robotic surgery bootcamp specifically designed for general surgery and subspecialty trainees, aligned with the realities of Canada’s healthcare system. A curriculum grounded in feasibility, scalability, and educational rigor has the potential not only to address local training gaps but also to serve as a scalable model for other institutions across Canada and in low-resource settings globally.
Methods
The robotic surgery bootcamp was developed as a collaborative initiative between faculty from the Division of General Surgery (colorectal, minimally invasive, bariatric, and hepatobiliary) and the Division of Urology at UofT (Figure 1). Bootcamp development began in 2022 following a review of existing literature on robotic surgical training curricula. This study protocol was considered a quality improvement project according to the University Health Network (UHN) Research Ethics Board and received an exemption by the UHN Review Committee (QI ID#22-0486).
Didactic component
The bootcamp included a 3-hour didactic session covering key topics in robotic general surgery, including colorectal, hepatobiliary, and hernia procedures. An additional session was delivered by a representative from Intuitive Surgical, outlining the company’s robotic certification process and highlighting international training opportunities.
Hands-on component
The hands-on training was based on published literature from urology, where robotic training is well established.16 Exercises were tailored to train novices in robotic surgery and designed to gradually increase in complexity, allowing participants to build upon previously acquired skills.
The session began with a 45-minute bedside introduction to the Da Vinci system, led by an Intuitive representative. Topics included robot docking, instrument handling and exchange, port placement, troubleshooting, and use of the console’s various functionalities.
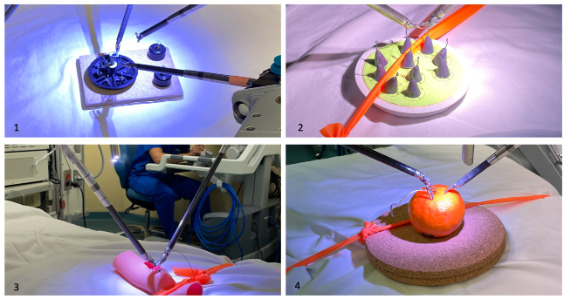
Participants were then divided into four pairs, grouped by similar baseline robotic skill levels. Each pair rotated through two hours of hands-on training at four stations. These included: Virtual simulation using Intuitive introductory modules and Progressive console-based tasks, including ring transfer, needle handling, suturing of synthetic bowel, and orange peeling (Figure 2). Each group is formed of only 2 participants to maximize training time and minimize idle time. Each 60-min hands-on block is subdivided into 30-min blocks of simulation and console training.
Assessment tools and Data collection
A pre-intervention questionnaire was administered on the day of the bootcamp to collect participant demographics, prior robotic surgery experience, baseline confidence, and knowledge of robotic systems. The same questionnaire was administered post-bootcamp, with an added section for feedback to inform future iterations. A copy of the survey is provided in Supplemental Digital Appendix A. The questionnaire was developed collaboratively by faculty with expertise in robotic surgery and surgical education at UofT. It was internally validated through iterative departmental review and pilot testing to ensure clarity, relevance, and content validity.
Participants rated their confidence using a self-assessed numerical scale from 0 to 10, where 0 indicated no confidence and 10 indicated full confidence in using the robotic system. Competence was assessed using a knowledge-based multiple-choice test that evaluated understanding of robotic system functionality, safety principles, and procedural steps. Scores were reported as the percentage of correct responses. Participants’ feedback was collected using Likert scale and open-ended questions.
Data Analysis
All continuous data were reported using means and standard deviations. The mean change in self-reported confidence and competence test scores pre- and post-intervention was analyzed using paired t-tests. Participants’ feedback including Likert scale responses, was analyzed using descriptive statistics, while open-ended responses were analyzed to identify recurring themes A p-value < 0.05 was considered statistically significant.
Results
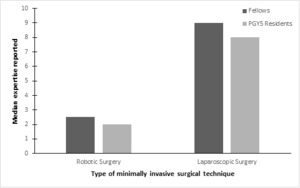
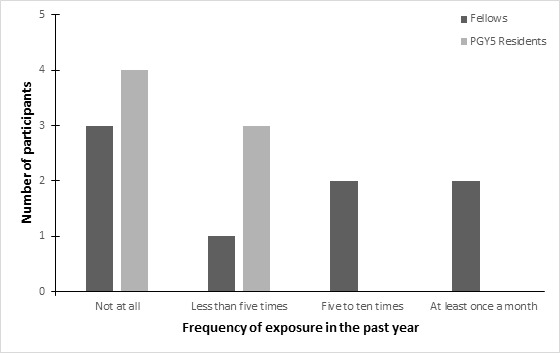
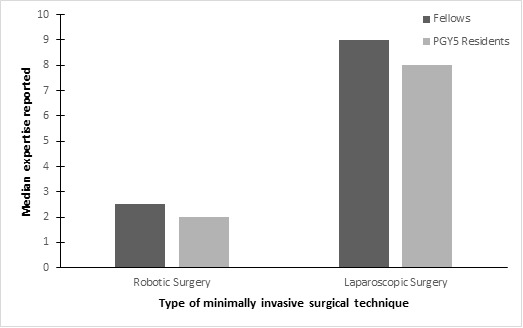
The bootcamp was conducted in January 2023 for eight fellows and in April 2023 for seven fifth-year residents. Pre-intervention survey results revealed that 7 (47%) participants had no exposure to robotic surgery in the past year, and 4 (27%) participants had fewer than five exposures. (Figure 3) The median self-reported baseline expertise in robotic surgery on a scale from 0 to 10 was 2 (range 0–4) for residents and 2.5 (range 0–9) for fellows. (Figure 4)
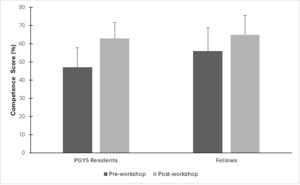
Post workshop results showed a significant improvement in the mean confidence levels for both fellows and residents. For fellows, the mean confidence increased from 3.1 (3.0) to 6.7 (1.4), p=0.002, while for residents, it increased from 2.0 (1.5) to 5.8 (0.9), p<0.05. (Figure 5) In terms of competence, fellows showed a non-significant improvement from 55.9% (13%) to 65.5% (10.06%), p=0.13. However, residents demonstrated a statistically significant improvement in competence, with scores rising from 47% (10.7%) to 63% (8.8%), p=0.03. (Figure 6)
Of all participants, 93% strongly agreed that they gained new knowledge from the course and felt the content was appropriate for their skill development. When asked about appropriate time to robotic surgery training, 87% of respondents indicated it should start during surgical residency. Open-ended feedback reflected overwhelmingly positive impressions of the bootcamp, with participants emphasizing the value of hands-on experience and immersive simulation. Many recommended developing a graded curriculum with staged skill progression, increased console time, and additional modules such as port placement and procedural simulations. All respondents strongly agreed that the course should be offered again.
Discussion
This robotic surgery boot camp represents the first of its kind for general surgery and its subspecialties in Canada. The program is innovative due to its condensed format, ease of deployment, cost-effectiveness, and its ability to meet the emerging demand for robotic surgery training among future general surgeons. Given the increasing use of robotic surgery across various surgical specialties, the need for formal, structured training is critical, and this boot camp offers a solution that addresses these needs efficiently.
A key strength of our robotic surgery boot camp was its low-cost, high-impact design, making it easily reproducible and scalable across training centers, including those with limited resources. The program was delivered over a single day using existing infrastructure at Toronto General Hospital. Importantly, all faculty volunteered their time, and both the Da Vinci Si simulators and consoles were made available on a weekend at no cost, eliminating barriers associated with access to expensive technology. Rather than relying on animal models or high-fidelity synthetic tissue, we used simple, reusable models (e.g., ring transfer, needle passing, synthetic bowel), which were low-cost yet effective in simulating key robotic tasks. This approach not only aligns with the ethical and logistical constraints of many institutions, particularly within publicly funded healthcare systems, but also supports more frequent and sustainable training opportunities. By leveraging institutional support, faculty engagement, and affordable simulation tools, programs can offer robust training in a format that is both educationally sound and widely accessible.
Our results, including overwhelmingly positive feedback and high participant satisfaction, indicate that the boot camp effectively increased trainees’ confidence in using robotic systems. While competence scores did not show uniform improvement, particularly among fellows, the significant gain in confidence is a key early outcome. For novice learners, increased confidence fosters continued engagement with training programs and is an essential first step toward developing technical proficiency17 Participants represented various training levels and general surgery subspecialties, supporting the program’s broad applicability. The iterative development of the boot camp, informed by participant feedback, will continue to refine the curriculum to meet the evolving demands of robotic surgery training. Moving forward, we aim to collaborate with national and international experts to further define and standardize the technical competencies required for robotic surgery. These competencies will be incorporated into Entrustable Professional Activities (EPAs)18 and milestones, providing a framework for assessing skill development in robotic surgery training. This framework will be designed with the constraints of publicly funded healthcare systems in mind, ensuring that the curriculum can be adopted globally while maintaining cost-effectiveness.
As part of the program’s long-term vision, we are exploring how to integrate this boot camp into residency and fellowship training programs. A comprehensive, longitudinal curriculum will include regular simulator practice, mandatory simulated modules (similar to the Toronto Urology Basic Skills Training Curriculum-BSTC) 19, and submission of videos of robotic-assisted operations for evaluation by senior colleagues. These recordings will be assessed using robotic Objective Structured Assessment of Technical Skills (r-OSATS),19 ensuring that training is aligned with high standards of surgical competence. We hope to bring together all Canadian program directors in acknowledging the importance of training future general surgeons in the latest robotic technique and hopefully offer similar training opportunities across all training programs.
However, there are limitations to our current study that should be acknowledged. The sample size was small, and the absence of long-term follow-up means we are unable to assess the durability of the improvements in confidence and competence. Additionally, while we measured immediate changes in confidence and competence, the effects of longitudinal training and skills assessments over time remain unclear. Future iterations of the program will aim to address these gaps by implementing follow-up assessments and developing a more robust longitudinal training pathway.
Conclusions
Robotic surgery is rapidly transforming the landscape of surgical practice, and training must evolve to meet this demand. Our bootcamp serves as a foundational model for cost-effective, scalable robotic education. While developed and implemented at a Canadian institution, the program is readily adaptable for integration into training curricula worldwide—particularly in regions where robotic training is still emerging, and resources are limited. With strong initial outcomes and high trainee engagement, this initiative lays the groundwork for a national robotic surgery training curriculum. Through continued development, expert collaboration, and integration into existing residency frameworks, we can ensure Canadian surgical trainees are equipped with the skills and confidence to lead in the era of advanced surgical technology.
Acknowledgments
The authors wish to thank our study coordinators, Nadia Rukavina, Aileigh Kay, and Roxana Bucur. We would also thank the University Health Network, Toronto General Hospital and The Temerty Advanced Surgical Education and Simulation Centre for their support in developing this program. No outside or industry funding was received for this project.
Ethical approval
This study was considered a quality improvement project according to the University Health Network (UHN) Research Ethics Board and received an exemption by the UHN Review Committee (QI ID#22-0486).
Funding/Support
None
Conflict of Interest
None
Other disclosures
None