INTRODUCTION
Injuries and disorders of the elbow may be treated by almost every subspecialty within orthopedic surgery. With shoulder and elbow, sports, hand, pediatric, and trauma fellowship-trained specialists routinely treating a wide variety of pathology of the elbow, adequate exposure to humerus/elbow procedures is essential during orthopedic surgical training. However, there is a large variability in the exposure to elbow cases in residency1
To monitor resident surgical exposure during training, the Accreditation Council for Graduate Medical Education (ACGME) operates a Resident Procedure Log System to which residents submit Current Procedural Terminology (CPT) codes after performing a procedure. In 2013, the ACGME established guidelines to define a threshold for the minimum number of core procedure experiences prior to graduation.2 The only case minimum requirement for elbow/humerus is 5 cases of supracondylar humerus percutaneous pinning3; however, this one case does not adequately reflect the variability of elbow pathology that may be managed in independent practice.
Sudah et al. analyzed the trends of elbow and shoulder surgery case logs and found a 4.4 fold difference between the 10th and 90th percentiles in procedure reporting elbow repair/revision/reconstruction cases and a 3.1 fold difference in fracture/dislocation cases in 2020, although their study is limited to data from 2016-2020.1 The primary purpose of our study was to evaluate trends of humerus/elbow procedure reporting by graduating orthopedic residency before and during the COVID-19 pandemic (2017-2022). We hypothesized that there would be a decrease in total procedures logged by residents graduating during the pandemic (academic years 2020-2021 and 2021-2022). The secondary purpose of this study was to assess how the procedure log guideline changes in 2013-2014 impacted the procedure numbers reported by residents. We hypothesized there would be an initial decrease in total humerus/elbow procedures after implementation secondary to a change in resident reporting practices, followed by a sustained increase in procedures during the years of the COVID-19 pandemic.
METHODS
We performed a retrospective review of graduating orthopedic surgery resident humerus/elbow procedure logs from 2006-2022. Institutional Review Board approval was not required due to the public availability of this anonymized data. Incision, Excision, Intro/Removal, Repair/Revision/Reconstruction, Trauma, Fracture and/or Dislocation, Manipulation, Arthrodesis, Amputation, Arthroscopy, Other, and Total procedure CPT codes for all patients (adult and pediatric) listed in the ACGME database were examined. We did not subgroup Intro/Removal, Arthrodesis, Amputation, Arthroscopy, or Other procedure categories despite their low sample sizes. Trauma procedures were excluded from analysis, as these represented a summation of already presented data and were only available for the 2007-2008 to 2015-2016 academic years.
Microsoft Excel spreadsheets (Excel, Microsoft Corporation, Redmond, Washington) were utilized to record and analyze humerus/elbow procedure data. Trends in procedures before and during the COVID-19 pandemic years (2017-2022) were examined using unpaired 2-tailed T-tests. An analysis of variance (ANOVA) was used to evaluate procedure minimums before and after implementation. The level of significance used in the ANOVAs and T-test for all humerus/elbow procedures was P<0.05. To compare across several procedure categories, P<0.005 was used in individual T-tests to protect against alpha errors.
RESULTS
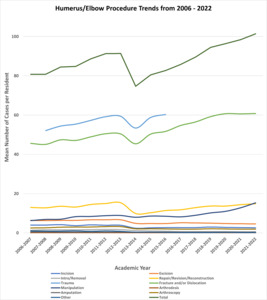
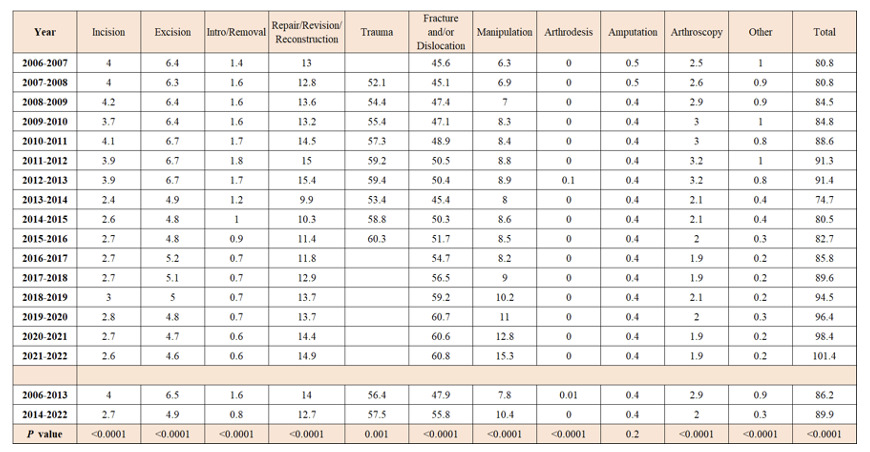
The mean volumes of all humerus/elbow procedures performed from 2006-2022 were tabulated and analyzed (Table 1). The mean number of all humerus/elbow procedures and categories reported by graduating orthopedic surgery residents demonstrated a significant increase in volume during the pre-pandemic academic years of 2017-2018 to 2018-2019 (89.6 vs 94.5, P=0.001). There were sequential years of non-significant growth until another significant increase was observed during the COVID-19 pandemic 2020-2021 and 2021-2022 academic years (98.4 vs 101.4, P=0.046, Fig. 1). Stratification of all humerus/elbow procedure categories demonstrated a significant increase during the academic years of 2019-2020 and 2020-2021 (11 vs 12.8, P=0.0004). Additionally, the significant increase in all humerus/elbow procedures during the COVID-19 academic years of 2020-2021 and 2021-2022 was primarily driven by humerus/elbow manipulation procedures (12.8 vs 15.3, P<0.0001, Fig. 2).
Significant differences in the mean volume of all humerus/elbow procedures before and after the implementation of minimum case log requirements (2006-2013 vs 2014-2022, Fig. 3) were analyzed using an ANOVA (Table 1). After case minimums were instituted, there was a significant reduction in Incision (4.0 vs 2.7, P<0.0001), Excision (6.5 vs 4.9, P<0.0001), Intro/Removal (1.6 vs 0.8, P<0.0001), Repair/Revision/Reconstruction (14.0 vs 12.7, P<0.0001), Arthrodesis (0.01 vs 0.0, P<0.0001), Arthroscopy (2.9 vs 2.0, P<0.0001), and Other procedures (0.9 vs 0.3, P<0.0001). A significant increase in procedure volumes after case minimums was observed for Fracture and/or Dislocation (47.9 vs 55.8, P<0.0001), Manipulation (7.8 vs 10.4, P<0.0001), and Total procedures (86.2 vs 89.9, P<0.0001). Amputations were the only procedures who did not demonstrate a significant change in volume when comparing these two time points (0.43 vs 0.40, P=0.2).
DISCUSSION
A retrospective review of ACGME orthopedic surgery resident humerus/elbow case logs from 2006-2022 revealed statistically significant increasing procedure volumes during the pre-pandemic academic years of 2017-2018 to 2018-2019 and again during the COVID-19 pandemic in academic years 2020-2021 and 2021-2022. We had initially hypothesized that the COVID-19 pandemic would negatively impact the consistent growth of humerus/elbow procedure logs, secondary to the cancellation of elective procedures for public health and safety. However, we observed increases in procedure reporting year over year from 2017-2022, during which time, a significant driver was the increase in manipulation procedures during 2020-2021 and 2021-2022 academic years.
During the COVID-19 pandemic, there were fewer patients presenting to the emergency department with elbow and upper extremity complaints than in the four proceeding years in the United States. Elbow and “upper arm” contusions, fractures, dislocations, and sprains were more likely to be admitted to the hospital, with all but elbow dislocations reaching statistical significance. Additionally, all age groups with elbow or “upper arm” injuries, except elbow injuries in the ages 0-20 were more likely to be admitted to the hospital during the pandemic than in the preceding years.4
In 2013, the ACGME implemented new guidelines for procedure logging. The new guidelines resulted in a decrease of case minimums, such as shoulder and knee arthroscopy.5,6 Similarly, we predicted a decrease in the volume of elbow procedures logged. However, the question remains whether the decreases seen in procedure logs is due to a true decrease in procedure volume or from a decrease in procedure logging once the minimum is met. For all surgical categories, there was a decrease in the number of procedure logs seen from 2013 to 2014, but a significant increase in procedure logging following the initial decrease from 2014-2019. However, while this increase has been significant, it only accounts for a 46% recovery from the initial decrease.7,8 We identified a decrease in Incision, Excision, Intro/Removal, Repair/Revision/Reconstruction, Arthrodesis/ Arthroscopy, and Other. There was an observed increased in Fracture and/or Dislocation, Manipulation, and Total procedures. Amputation remained unchanged.
The largest limitation of our analysis is that it relies on self-reported and manually entered data from residents and is compiled and reported in the graduation year of each resident. Procedure numbers associated with ACGME case logs are highly variable due to a lack of standardization in procedure logging practices and may not accurately reflect a resident’s procedural experience.9 While this variability exists, orthopedic surgery residents log cases with higher accuracy than residents in general surgery and neurosurgery.10 Furthermore, a graduating resident has compiled 5 years of data over the course of residency, and we are unable to determine based off the dataset when the codes were logged. Additionally, we did not stratify by pediatric or adult procedure types. The analysis of the impact of the pandemic is also limited as we only analyzed two academic years. Future analysis of the pandemic’s continued impact should be followed to determine the impact of COVID-19 on orthopedic resident surgical training.
Additionally, the 2020 ACGME merge with the Association of American Colleges of Osteopathic Medicine (AACOM) and the American Osteopathic Association (AOA) may have a cofounding effect on the results for the 2020-2021 academic year. This was the first time both allopathic and osteopathic orthopedic programs had data coded in the same system, and the possible effect this could have on reporting has yet to be determined.11
CONCLUSION
A retrospective review of graduating orthopedic surgery resident reported ACGME humerus/elbow cases logs from 2006-2022 revealed significant increase from 2017-2022 except for the 2019-2020 academic year. Manipulation procedures were a significant driver during the 2020-2021 and 2021-2022 academic years. Orthopedic surgery residents continued to report increases in humerus/elbow procedures throughout the pandemic.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflicts of interest.
ETHICS STATEMENT
Institutional Review Board (IRB) approval was not required for this study as it utilized publicly available, de-identified data from the Accreditation Council for Graduate Medical Education (ACGME) case log system. No human subjects were involved, and no patient consent was required.